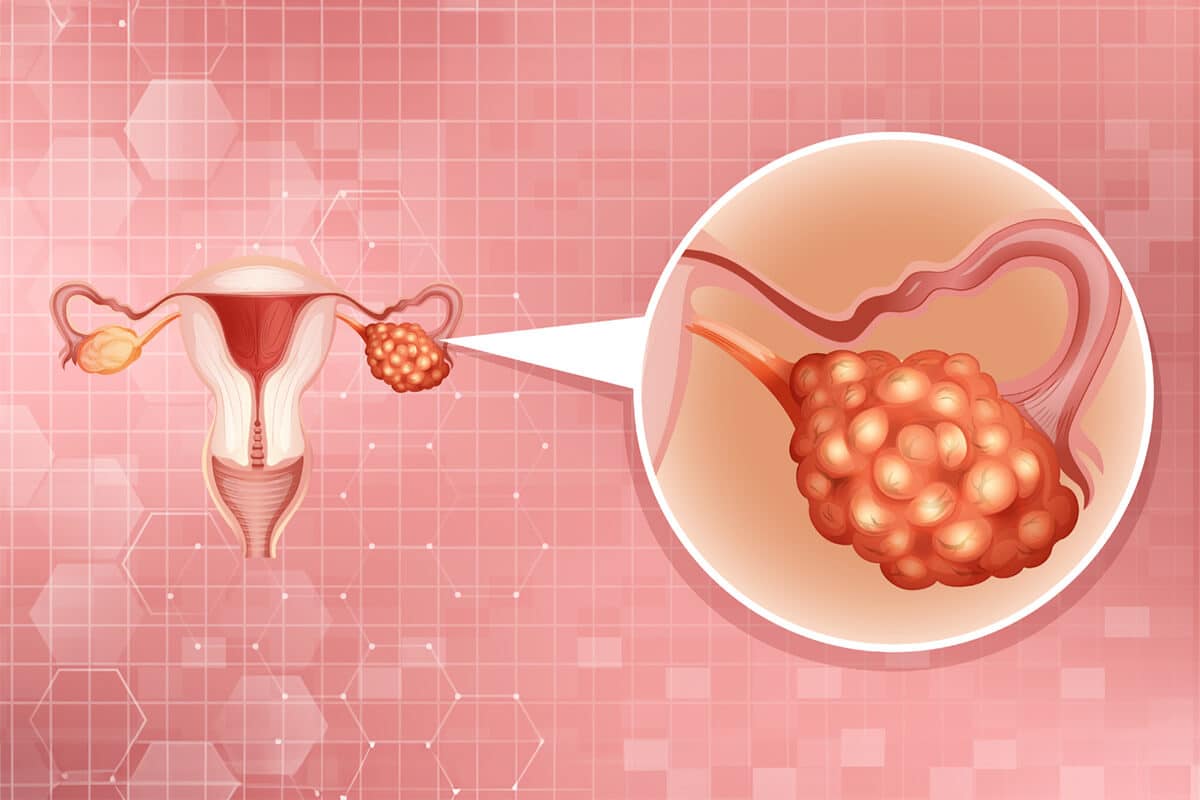
Targeting homologous recombination deficiency in ovarian cancer
Maintaining genomic integrity and preventing cell death requires a complex network of molecular repair pathways, as DNA damage is a constantly occurring event (Frey et al., 2017).
Homologous recombination (HR) is a repair process, which plays an important role in repairing double-stranded DNA breaks (DSBs) (Frey et al., 2017). When HR is deficient, cells are relying on other, less precise and more error-prone repair pathways such as the non-homologous end-joining (NHEJ) pathway, which leads to the accumulation of additional mutations, genetic aberrations, copy number alterations, and chromosomal instability leaving an irreversible „genomic scar” (Frey et al., 2017; Li et al., 2020).
An increased risk of cancer is associated with acquired or inherited defects in DNA repair pathways (Ledermann et al., 2016). According to The Cancer Genome Atlas (TCGA) project, ~50% of high-grade serous carcinoma (HGSC), which is the deadliest form of epithelial ovarian cancer, exhibit homologous recombination deficiency (HRD) (Ngoi & Tan, 2021). In the context of HGSC, HRD derives from pathogenic germline/somatic variants and epigenetic modifications in either BRCA1/2 or in genes encoding for key players in the homologous recombination repair (HRR) pathway. Alterations in RAD51B/C/D, PALB2, ATM, H2AX, CHK1/2, CDK12, NBN, MRE11, RPA, BRIP1, BARD1, RAD51, Fanconi Anemia genes, PTEN, and EMSY have been shown to potentially confer an HRD or BRCAness phenotype, which is characterized by deficiencies in the DSB repair pathway (Magliacane et al., 2022). The term BRCAness describes tumors that have not derived from a germline BRCA1 or BRCA2 mutation, however, the phenotypes are similar to these hereditary cancers (Lord & Ashworth, 2017).
HRD-positive tumors respond well to platinum-based chemotherapy and poly (ADP-ribose) polymerase inhibitors (PARPis) (Iglehart & Silver, 2009). The latter represents a precision oncology approach, a new trend in the treatment of ovarian carcinomas, and the indications for which PARP inhibitors are approved have been expanding in recent years. Currently, three PARP inhibitors are approved by the U. S. Food and Drug Administration (FDA) in settings such as primary maintenance or switch maintenance therapies, as well as for the treatment of patients with BRCA mutations or HRD positivity (Virani et al., 2021).
Pharmacological PARPis have two general effects, one of them is catalytic inhibition of PARP1/2 via preventing PARylation, and another one is ‘trapping’ PARP1/2 on damaged DNA, this latter effect being responsible for much of the tumor cell cytotoxicity caused by these drugs (Luo & Keyomarsi, 2022; Krastev et al., 2021).
PARPis have been developed based on their predicted synthetic lethality in the context of HRD-positive cells (Ngoi & Tan, 2021). Synthetic lethality is a concept that describes the situation where a defect in either one of two genes has little effect on the cell or organism but a combination of defects in both genes results in death (Lord & Ashworth, 2017). When the cell functions normally, both base-excision repair and HR mechanisms are available for DSB repair. Even in cells where one of the repair mechanisms is nonfunctional – either because of a mutation in the HR pathway or because of PARP1 inhibition – the other, intact DNA-repair mechanism can repair DNA damage. However, in HRD-positive cancer cells, when the base-excision repair is inhibited by PARPi and HR pathways are dysfunctional to begin with, the cell is unable to repair the DNA damage which results in cell death (Iglehart & Silver, 2009).
PARPis frequently elicit a good initial response, although most patients develop resistance to these agents, resulting in disease relapse (Dias et al., 2021). There are different mechanisms through which resistance can occur, such as altering the tumor microenvironment through hypoxia, the presence of agents (for instance PI3Kinase inhibitors) that can down-regulate HRR (Ledermann et al., 2016), inactivation of the DNA repair proteins, which leads to the restoration HRR and loss of a number of proteins, including PARP1 as well. There are also so-called secondary „revertant” mutations in BRCA1 or BRCA2 genes, which can restore sufficient HRR function and lead to PARPi resistance (Lord & Ashworth, 2017).
Repeated sequencing of tumors may help to detect the reversion mutations; however, real-time testing requires repeated sampling time points, in this context, liquid biopsy could be a suitable approach that is deservedly being explored in ongoing trials (Ngoi & Tan, 2021).
Currently, there are several commercially available assays based on liquid biopsy which target HRD for prediction of the sensitivity to PARP inhibitors. BRACAnalysis CDx and FoundationOne Liquid CDx are FDA-approved assays that detect potential causes of HRR impairment. The Resolution HRD assay, a companion diagnostic for the PARP inhibitor Niraparib from Resolution Bioscience, Inc., detects gene deletions from cell-free DNA and differentiates between single copy and biallelic gene deletions.
The Epic Sciences CTC HRD assay from Epic Sciences, Inc., measures chromosomal instability, which is a hallmark of cancer and has also been associated with DNA damage repair, within circulating tumor cells. Predi-HRD liquid biopsy test provides real-time monitoring of tumor heterogeneity over time and highly sensitive detection of homologous recombination gene defects.
There are also ongoing clinical trials that evaluate the combination of therapies to overcome PARPi resistance and enhance PARPi sensitivity, however, it must be noted that a combination treatment often involves more severe toxicity profiles. Promising possibilities are represented by combining PARPis with anti-angiogenic agents, immunotherapy, PI3K/AKT pathway inhibitors, Ras/Raf/MEK/MAPK pathway inhibitors, ATR/WEE1 inhibitors or epigenetic modifiers (Giudice et al., 2022).
In conclusion, based on the ongoing preclinical trials, PARP inhibition is a technique that is under active research, with the following areas in the focus: fighting against drug resistance via identifying the mechanisms that cause PARPi resistance and biomarkers that predict it, optimizing combination therapy and identifying the target treatment population (Lord & Ashworth, 2017).
References
- Frey, M. K., & Pothuri, B. (2017). Homologous recombination deficiency (HRD) testing in ovarian cancer clinical practice: A review of the literature. Gynecologic Oncology Research and Practice,
- Li, H., Liu, Y., Wu, N., Chen, C., Cheng, Q., & Wang, J. (2020). PARP inhibitor resistance: The underlying mechanisms and clinical implications. Molecular Cancer, 19.
- Ledermann, J. A., Drew, Y., & Kristeleit, R. S. (2016). Homologous recombination deficiency and ovarian cancer. European Journal of Cancer, 60, 49–58.doi:10.1016/j.ejca.2016.03.005
- Ngoi, Y. L., & Tan, S. P. (2021). The role of homologous recombination deficiency testing in ovarian cancer and its clinical implications: Do we need it? ESMO Open, 6(3).
- Magliacane G, Brunetto E, Calzavara S, Bergamini A, Pipitone GB, Marra G, Redegalli M, Grassini G, Rabaiotti E, Taccagni G, Pecciarini L, Carrera P, Mangili G, Doglioni C, Cangi MG. Locally Performed HRD Testing for Ovarian Cancer? Yes, We Can! Cancers (Basel). 2022 Dec 21;15(1):43. doi: 10.3390/cancers15010043. PMID: 36612041; PMCID: PMC9817883.
- Lord, C. J., & Ashworth, A. (2017). PARP Inhibitors: The First Synthetic Lethal Targeted Therapy. Science (New York, N.Y.), 355(6330), 1152.
- Iglehart JD, Silver DP. Synthetic lethality–a new direction in cancer-drug development. N Engl J Med 2009;361:189–91.
- Virani S, Baiocchi G, Bowtell D, Cabasag CJ, Cho KR, Fortner RT, et al. Joint IARC/NCI International Cancer Seminar Series Report: expert consensus on future directions for ovarian carcinoma research. Carcinogenesis 2021;42:785–93.
- Luo, L., & Keyomarsi, K. (2022). PARP inhibitors as single agents and in combination therapy: The most promising treatment strategies in clinical trials for BRCA-mutant ovarian and triple-negative breast cancers. Expert opinion on investigational drugs, 31(6), 607.
- Krastev DB, Wicks AJ, Lord CJ. PARP Inhibitors – Trapped in a Toxic Love Affair. Cancer Res. 2021 Nov 15;81(22):5605-5607. doi: 10.1158/0008-5472.CAN-21-3201. PMID: 34782321.
- Dias, M. P., Moser, S. C., Ganesan, S., & Jonkers, J. (2021). Understanding and overcoming resistance to PARP inhibitors in cancer therapy. Nature Reviews Clinical Oncology. doi:10.1038/s41571-021-00532-x
- Giudice, E., Gentile, M., Salutari, V., Ricci, C., Musacchio, L., Carbone, M. V., Ghizzoni, V., Camarda, F., Tronconi, F., Nero, C., Ciccarone, F., Scambia, G., & Lorusso, D. (2022). PARP Inhibitors Resistance: Mechanisms and Perspectives. Cancers, 14(6).
Recent blogs
Cell-free DNA Fragmentomics: A Promising Predictor of Cancer
In this blog entry, we will explore the recent history, intriguing findings, and tools related to cfDNA fragmentomics.
New developments in the field of circulating tumor cells (2024)
The blog post focuses on how researchers can produce more meaningful, applicable results that directly benefit human health.
Singlera technologies 5: Panseer – detecting pan-cancer signatures years before conventional diagnosis
In the last blog of the year and the concluding chapter of the Singlera series, we are going to explore PanSeer, a blood-based screening test utilizing unique methylation signatures.